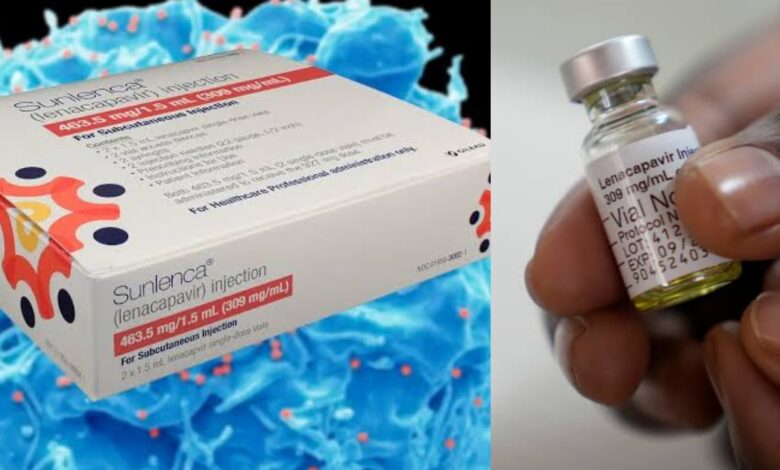
Scientists have created a powerful new weapon against HIV: a simple injection that protects you for six months with just two shots a year. Called Yeztugo (Lenacapavir), this breakthrough drug is 99.9 per cent effective at stopping HIV infection, according to major trials in Africa.
Developed by Gilead Sciences and approved by US regulators on June 18, 2025, Lenacapavir has been hailed as a revolutionary PrEP option, especially for populations unable to adhere to daily oral pills due to stigma, forgetfulness, or access issues in what has been hailed as ‘Breakthrough of the Year’ by Science magazine.
“This is the transformative PrEP option we’ve been waiting for,” said Dr Carlos del Rio of Emory University and explained that the two shots a year solve the big problems with daily pills – people forget to take them or face stigma, besides studies showing most people prefer fewer doses.
In October 2024, Gilead struck deals with six generic drug makers to produce cheaper versions of Lenacapavir for 120 poor countries. The company promised to sell the drug at cost price until these manufacturers can supply enough doses globally.
Kenya is among 18 priority countries to get Lenacapavir, a revolutionary option for populations unable to adhere to daily oral pills due to stigma, forgetfulness or access issues.
With 17,000 new infections and 21,000 AIDS-related deaths reported in Kenya in 2023 alone, the fight is far from over. Luckily, Kenya is among 18 priority countries getting the drug first for being among those that account for 70 per cent of HIV cases in eligible countries.
Despite its promise, the price tag for Lenacapavir has raised alarm. Gilead is expected to charge about $28,218 (Ksh3.6 million) per patient annually in the US, an amount that is inaccessible for most low- and middle-income countries (LMICs), where HIV treatment costs on average just $75 (Ksh9,680) a year.
However, research from Dr Andrew Hill in the University of Liverpool suggests that Lenacapavir could be produced for as little as $25 (Ksh3,226) a year if manufactured generically and at scale.
As Kenya considers the rollout of Lenacapavir, the twice-yearly injectable PrEP, the big question remains: Can the health systems in remote areas support this innovation, and can the people who need it most actually access it?
Poor infrastructure, long distances, and unreliable power supply compromise storage and delivery of life-saving medicines.
Kenya is among 18 priority countries to get Lenacapavir, a revolutionary option for populations unable to adhere to daily oral pills due to stigma, forgetfulness or access issues.
As Kenya considers the rollout of Lenacapavir, the twice-yearly injectable PrEP, the big question remains: Can the health systems in remote areas support this innovation, and can the people who need it most actually access it?
Poor infrastructure, long distances, and unreliable power supply compromise storage and delivery of life-saving medicines.





